Quartet's platform and services drive value where it matters most, for you and for your members
One platform for all your mental health needs, across all lines of business
Quartet covers everything from reaching your members and connecting them to the right mental health care, so that they can focus on what matters: their health.
Support value-based mental health care
We’ll work with you to develop, implement, and track the quality of mental health in your network, so you can be confident your members are not only getting the care you’re paying for, but what they deserve.
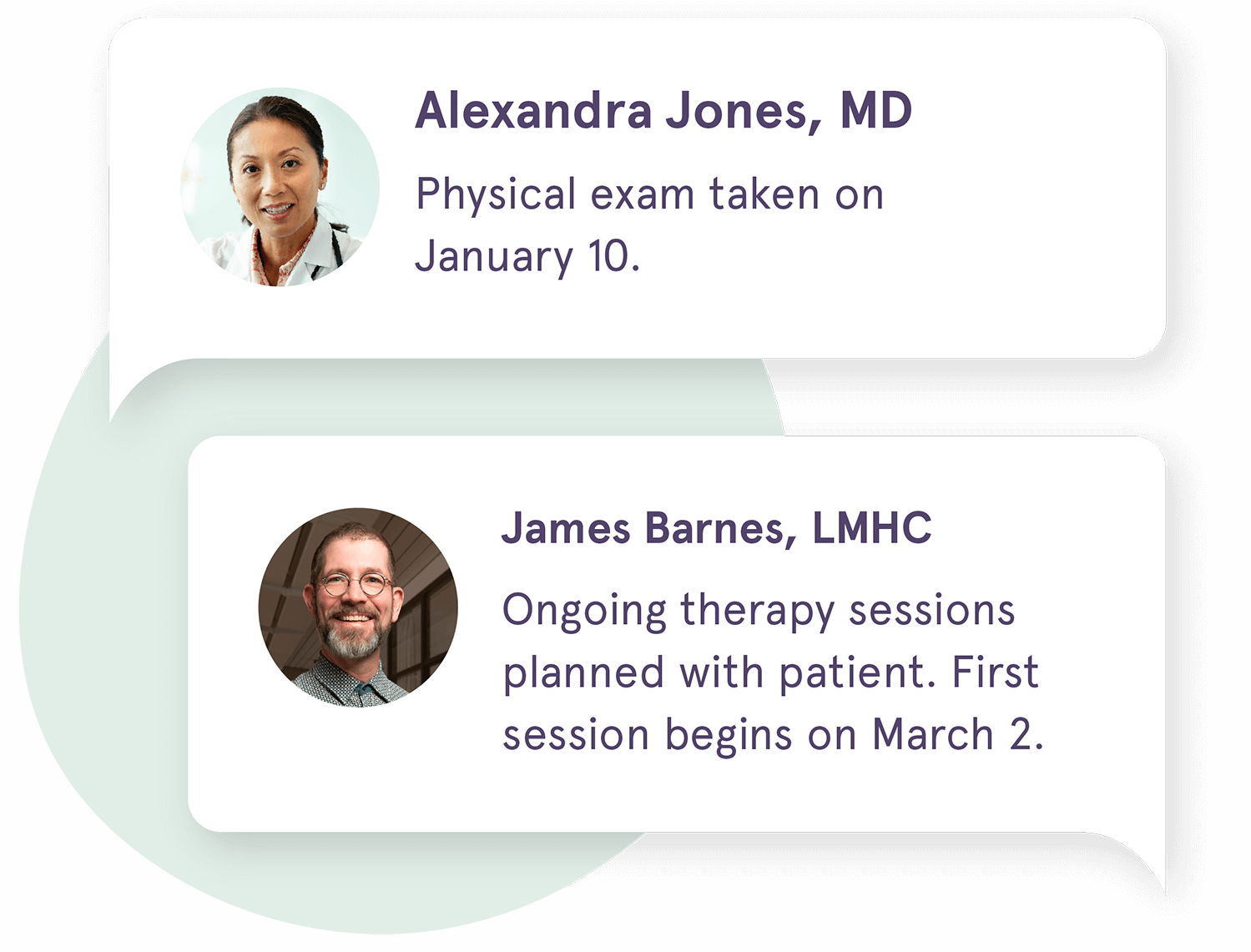
Seamless workflow integration
Our platform can be integrated into your referring providers’ workflows, fostering efficient communication and collaboration at scale.
Meaningful returns
You’ll receive a strong ROI through cost of care savings, improved market share, and optimized utilization patterns.
How Quartet helps your members
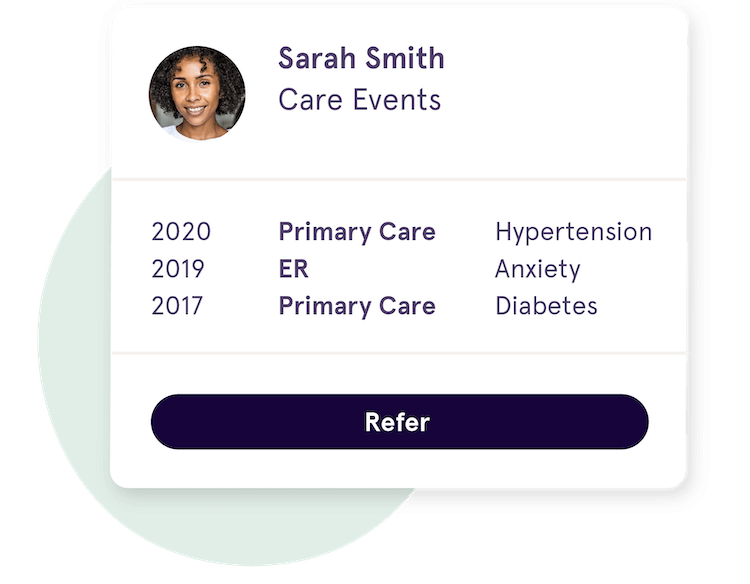
Proactive patient screening
Generate insights about patients’ health, to learn more about who may need proactive support.

Mental health care access
Your members can access mental health care through a referral from a provider or case manager, or sign up directly themselves. We then match them to care that meets their needs, preferences, and insurance.
A collaborative care team
Physicians and mental health providers can work together and stay up to date on a member’s progress and treat total health.
Personalized care
Members can select care preferences, answer questions about their health, request a new provider match, and more.
Support along the way
Our team of Care Navigators provide support and guidance along your members’ care journeys.
Health Insurance Plan Partners
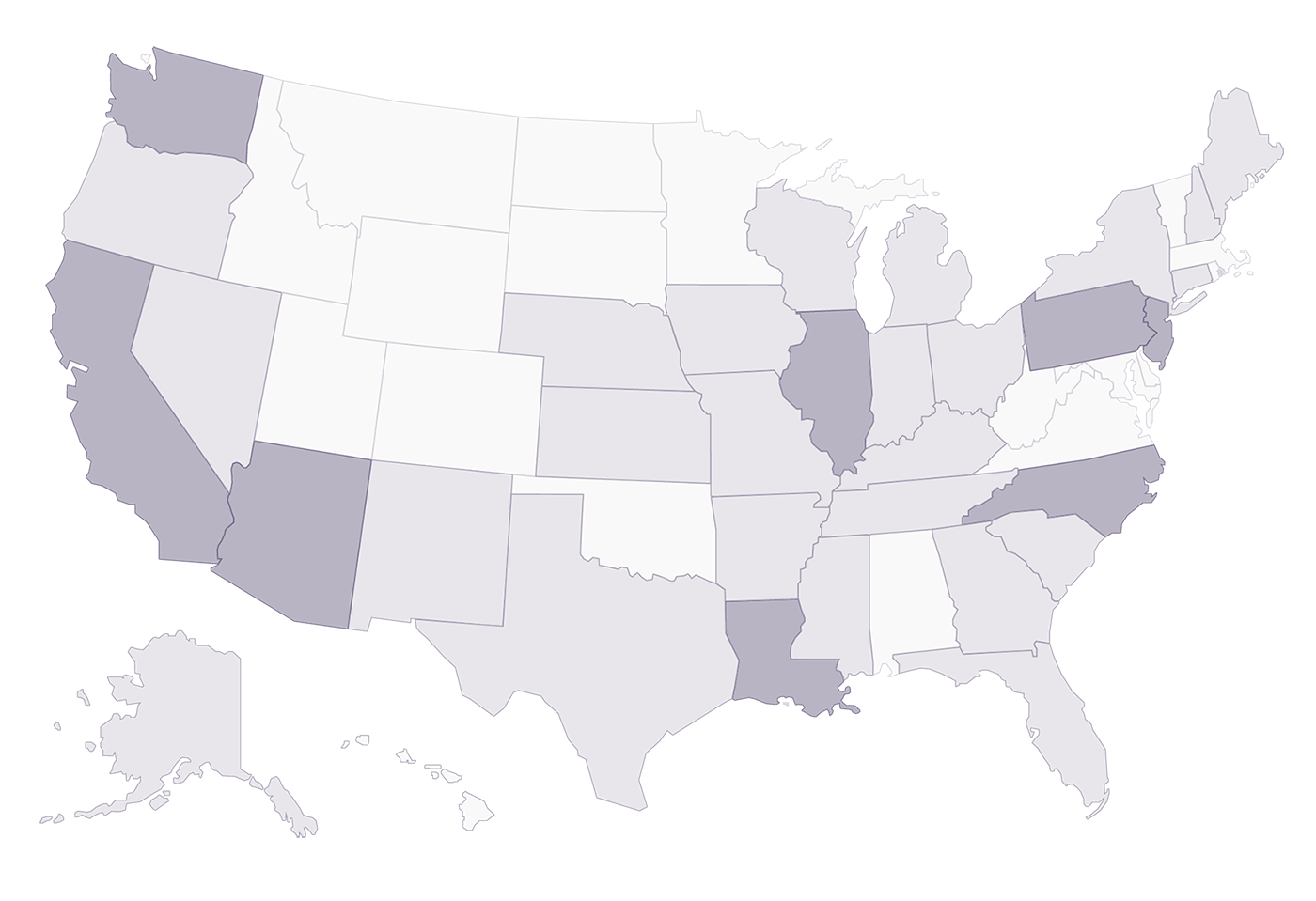
Join health plans nationwide
We work with health plans and delivery systems around the country to drive improved mental health outcomes. We currently work in the following markets, and below are some of our partners.
Improve your members' health and cost outcomes
Sign up to receive more information from our team, or email [email protected].
Frequently asked questions
Who are your current enterprise partners?
Quartet partners with national and regional health plans and health care delivery systems across all lines of business. Some of our plan partners include Centene Corporation, Regence (Washington), Horizon Health Systems (New Jersey), and Sutter Health (California).
How do you structure your partnerships, and what ROI can health plans expect?
Our partnerships are structured to maximize value creation and drive an increase in quality of care to enable better outcomes. We offer an enterprise SaaS (software as a service) agreement structured over a five-year period with annual fees, across commercial, Medicare Advantage and Medicaid lines of business. The pricing model is structured to drive significant ROI across the life of each health plan partnership.
What does your implementation process and timeline look like for health plan partners?
We work with health plans to meet their unique mental health care needs and complement existing initiatives. Once we sign a partnership, Quartet works closely with the plan partner to design and implement a strategy to launch in the market. This includes analyzing data, recruiting mental health providers to accept patients from Quartet, and getting referring providers to begin using the Quartet platform. We work quickly to learn and understand a market so that we can connect members to the right mental health care right away. Our solution is easy and ready-to-use, requiring little technical lift from referring providers or systems to get started.
What results have you seen with partners?
Quartet’s program has resulted in total cost of care reduction for health plan partners, driving savings of >$100 per engaged member per month for a mixed population of Medicare Advantage, commercial, and ACA members.
What are Quartet's virtual care options?
Quartet connects members to the best care for them, based on needs, preferences, and insurance. We match to a robust network that includes in-person and tele mental health care (therapy and psychiatry), and digital care options like computerized Cognitive Behavioral Therapy (cCBT). Quartet will help onboard a health plan’s existing mental health provider network to be used as telehealth care options. Quartet has a designated team to evaluate digital care options via market landscaping, rigorous clinical vetting, and running lean pilots across multiple markets. We also have a provider engagement team that supports mental health care providers work with Quartet, and a team of clinical advisors who evaluate the efficacy and quality of care options.
Does Quartet work within a health plan's network?
Yes, Quartet works with a health plan’s existing network. Where network gaps are identified, Quartet will recruit mental health providers (both prescribers and non-prescribers) to ensure we can meet member demand. If there are provider groups we believe will improve a plan’s network, we’ll establish a process to surface them for expedited credentialing and contracting.