Innovation Through Alternative Payment Models: Working With Commercial Payers to Support Patients With Serious Mental Illness

May 14, 2024
Quartet Health, in collaboration with Blue Cross Blue Shield Michigan (BCBSM) and Easterseals MORC, recently led an enlightening panel at NatCon24, focusing on the transformative potential of alternative payment models in behavioral health for patients with serious mental illness (SMI).
Quartet Health President and Chief Operating Officer, Anay Patel, moderated the panel, alongside BCBSM and Blue Care Network Director of Behavioral Health Strategy and Planning, Julia Isaacs, and Easterseals MORC Senior Vice President and Chief Program Officer, Juliana Harper.
The Challenge and the Innovative Response
Commercially insured members in Michigan, especially those diagnosed with SMI like bipolar disorder, schizophrenia, or major depression (which represent 1 in 5 behavioral health conditions), have historically faced limited options for behavioral health care. It was stated that, historically, in Michigan,commercially insured members had even fewer care options than those who are uninsured. And while telebehavioral health workforce development solutions like innovaTel Telepsychiatry help alleviate the pressure on care delivery organizations, the ever-present behavioral health provider shortage (especially for those able to treat SMI) only adds to the challenges.
Additionally, inpatient admission rates and total spend of behavioral health patients with co-occuring mental health and substance abuse conditions were five times that of other behavioral health patients, with 18K+ behavioral health adverse events (including suicide, self-harm, or overdose) reported. “There wasn’t anything that was serving this patient population well. Care coordination and case management programs were siloed and fragmented,” said Harper.
In response, the panel discussed the creation of the Adult Intensive Service (AIS) program, an initiative designed to provide a public mental health perspective to a private insurance framework, bridging significant care gaps. Many of the services the AIS program incentivizes were previously limited or not available for SMI patients through a comprehensive payment model, especially as it relates to wraparound care for the commercially insured population.
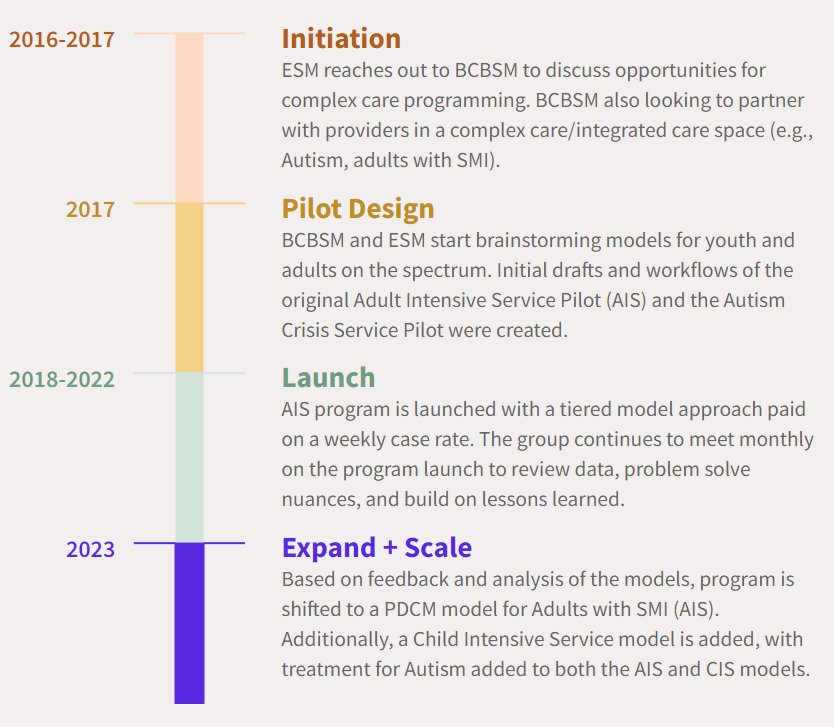
Program Timeline
4 P’s of the AIS Program
- Population
-
-
- Adults or children with SMI/serious emotional disturbance (SED), mood disorders, psychotic disorders, co-occurring substance use, and Autism Spectrum Disorder (ASD)
-
- Program Services
-
-
- Fast access to care
- Comprehensive ASD evaluation completion
- Care coordination and case management
- Social determinants of health (SDoH) support, peer support, and parental support
- Personalized treatment plans
-
- Performance
-
-
- Average time to services
- Average time from intake to first appointment
- Current satisfaction with services
-
- Payment
-
- Provider-Delivered Care Management (PDCM) codes
- 99847: First hour billed monthly
- 99489: Subsequent 30 minutes billed monthly
- Fee-for-service (FFS) schedule supporting in-scope psychiatric and therapy services
- No pre-authorization requirement for qualifying providers
- Provider-Delivered Care Management (PDCM) codes
Meaningful Outcomes
The AIS program has been instrumental in achieving remarkable improvements in patient care and cost efficiency. Some of the impressive outcomes highlighted include:
- Rapid Access to Care: The program has reduced the average time from referral to outreach to just one day, and from intake to treatment to less than one week, even more impressive when compared to the 30-40 day time-to-care for SMI patients reported in other markets.
- Year-over-Year Growth: There has been a 2.5x increase in patients engaged year over year (YoY) from 2022 to 2023.
- Enhanced Safety and Satisfaction: There was an 8% decrease in adverse events YoY, alongside a 97.5% member satisfaction rate, demonstrating both the safety and effectiveness of the care provided.
- Reduced Inpatient Admissions: Less than 10% of engaged members were admitted to inpatient care, reflecting the program’s success in managing care in less restrictive environments.
Leveraging Collaborations and Alternative Models
Anay Patel, President and COO at Quartet Health, emphasized the need for innovative solutions, noting, “We’re seeing more collaboration between payers and providers to meet the needs of acute behavioral health patient populations, especially those with serious mental illnesses. There’s a needed paradigm shift towards incentivizing services that improve access to care and total cost of care, not at the expense of costlier care.” This collaborative spirit is central to the AIS program’s success and is vital for its future expansions. Patel later added, “AIS is a fantastic example of how to start along a glide-path with alternative payment models. As payers and providers start to see scalable outcomes, they can collaboratively move along the continuum of structured risk models.”
Juliana Harper, Senior VP and Chief Program Officer at Easterseals MORC, discussed the critical nature of partnerships, stating, “It all started by building relationships and staying persistent.” She further highlighted the effectiveness of team-based care: “Team-based care is engaging and leads to clinician and patient satisfaction.”
Julia Isaacs, Director of Behavioral Health Strategy and Planning at BCBSM, underscored the value of alternative payment models, “The spirit of this alternative payment model is that we want to make sure we cover services that are not usually covered in traditional commercial insurance.” And what’s more? “When we expand services, we see cost savings.”
The Future of Behavioral Health Care and What’s Next
The future of these alternative payment models looks promising, with plans to further refine and expand these strategies. Isaacs shared the vision for the evolution of these models: “We’re looking for partners, not just providers. You’re likely already providing these services to your patients; you’re just not getting paid for it. We want to pay you for it.”
Harper had this advice to those interested in implementing similar models: “We didn’t wait for the payers to come to us; we went to them. Find your people and be persistent.”
Isaacs echoed this sentiment, also emphasizing the need for program education: “We need partnerships and risk arrangements to help facilitate physical and behavioral health integration. It’s not about ‘if you build it they will come.’ If you build it, they don’t know you built it. There’s an educational component to this.”
The panel at NatCon24 highlighted the significant strides being made in behavioral health through innovative payment models. The AIS program and similar initiatives represent pivotal advancements in making behavioral health care more accessible, effective, and efficient. By continuing to adapt and expand these models, we can ensure a more robust and responsive health care system that better serves individuals with SMI and enhances overall community health.
Explore more

Quality Mental Health Care, Wherever You Are
At Quartet, we know that mental health care isn’t one size fits all.

Take Your Own Advice: A Note to Therapists on Self Care During COVID‑19
COVID-19 added a layer of complexity for mental healthcare workers, who may be experiencing their own stressors and anxieties related to the crisis.

Fighting Two Pandemics: Supporting Domestic Violence Survivors and Their Mental Health Needs During COVID‑19
For some, following the stay-at-home orders for one pandemic may render them vulnerable to another: domestic violence.



